More Mysteries- Finding Klinefelter’s
While seeking answers to advocate for myself, I’ve been doing a lot of research. The need to seek out answers and solutions is an immutable component of my character.
So, it’s no surprise really that I see the puzzles like mine in those I am near.
Long before I started piecing together my Ehlers-Danlos puzzle, someone very special to me (let’s call him Joey) was also seeking answers to his equally cryptic puzzle.
In fact, many of our symptoms overlap, and I’ve found myself often thinking, “Are we sure he doesn’t have EDS too?”
He’s not hypermobile, which has been the cornerstone of me getting care, so I had to keep looking.
He’s been to SO MANY doctors. He started seeking medical help with his overall state of being in 2019, before COVID-19 halted everything.
He’s had endoscopies, colonoscopies, been referred to endocrinologists, allergists, a sleep clinic, pulmonologist, bariatric, urology and I’m probably honestly missing some.
Which SCRIPTs are you stuck in?
Starting the Search
In 2021, he was overheating all of the time. He was overheating when it was 50 degrees out, and stepping out into -17 degree temps without a shirt, wearing shorts to try to cool off. He was miserable in the summer.
Once again, Dr. Facebook was our first real help.
I was reading accounts on my timeline of trans women feeling colder from taking estrogen, and trans men feeling hotter on testosterone, so he requested his GP (we shall call him Dr. Hardon) test his estrogen.
Dr. Hardon explained how testosterone-estrogen conversion occurs, and he ordered a testosterone lab.
Labs
Joey’s testosterone (T) levels were low. They were so low they were nearly nonexistent.
I now know that Joey’s testosterone levels, paired with his hypogonadism, should have immediately triggered a screening for Klinefelter’s syndrome. Despite screening criteria being clear in the research about KS, no such practice exists.
KS went without mention, and he was referred to his first Endocrinologist, Dr. Bridenstine with Banner Health here in Northern Colorado. (He now works for UC Health in Longmont and I’m using his real name because anyone seeking help needs to be warned.)
Endocrinology
Dr. Bridenstine, despite seeing the very low T levels, despite the presence of hypogonadism, which he verified himself, told Joey that he should stop listening to radio commercials hoping for a bigger boner, and tried to talk Joey out of trying T therapy.
During this appointment, Joey was wholeheartedly dismissed, and had to beg for help.
Dr. Bridenstine should have ordered a karyotype test that same day. He did not. He didn’t mention it at all.
He referred Joey to a urologist, because in addition to overheating all of the time, Joey also has to use the bathroom upwards of 20 times a day. He also ordered an ultrasound of Joey’s testicles, to make sure they exist, because they could not be located during the exam.
He started Joey on weekly injectable T, and strongly urged Joey to be screened for Sleep Apnea which can interfere with treatment.
Joey started the T and was able to raise his testosterone to the low normal range! Joey also became polycythemic, and had to stop testosterone therapy.
Urology
Joey had the ultrasound, where they couldn’t find blood flow to his testes, and went to the urologist, Dr. Wolach also with Banner Health (also his real name).
During this visit, Dr. Wolach told Joey that the structural anomaly was the result of development, and that had it been caught in his teens they may have had some options, but that absolutely nothing can be done structurally now. Dr. Wolach told Joey he had retractile testes.
He blamed the frequent urination on soda consumption (Joey quit drinking soda 3 months ago, and still pees all day).
He said this was just how Joey developed, and discouraged him from seeking further answers.
According to the internet, retractile or undescended testicles can be treated surgically.
Cambridge University says,
“A small incision is made in the groin to free the muscle retracting the testis so that it can be brought down into the scrotum. A second incision is then made in the scrotum to receive the testis where it is anchored to prevent twisting and further retraction.”
For some reason, Dr. Wolach decided to close that door and dismiss Joey instead. I just want to point out that this is an awful lot of humiliating poking and prodding just to hit a brick wall.
Sleep Apnea
Joey continued to advocate for himself. He was diagnosed with obstructive sleep apnea, and started using a CPAP.
Trudging Forward
This enabled him to restart T, but this time in the form of the gel.
Despite therapy for a variety of symptoms, many of the symptoms were getting worse.
Trying to Access Care
When Joey first approached his GP with his list of symptoms, Dr. Hardon said he could only address one thing at a time, and that Joey would need to make repeated trips to address the rest. He’s been going about monthly for 3 years now.
Dr. Hardon refused to look at the list as a combined presentation. He looked at one symptom at a time, and would test/prescribe/refer for each symptom, citing the 15-minute visit limitation as the barrier to holistic care.
I have felt very deeply from the beginning, that each of these symptoms are only part of a larger syndrome or disorder. Dr. Hardon wasn’t going to look for it, and endocrinology and urology refused as well.
If Joey hadn’t had Medicaid, I have no idea how he would have been able to continue after so many practitioners have utterly refused to see this.
I dug deeper. I searched and searched for a combined answer.
Klinefelter’s Syndrome
I had learned about Klinefelter’s syndrome in college, but only in passing. When taking biology they taught that there were two sexes, male and female… except that there’s this long list of natural variations that do not fit into that binary, and that binary is much more like a spectrum. The second half of that statement was presented more like a whisper.
When I started digging into the information about Klinefelter’s it was like being hit with a brick. Klinefelter’s syndrome affects absolutely everything, and none of the doctors were looking at everything.
Most of the information I found was from overseas. Study after study said the same things. This is fairly common (1 in 600) but very rarely diagnosed (25%). In children it is found when the symptoms are severe. In adults it is found when men seek fertility treatment (which is quite expensive). This leaves some very obvious gaps.
According to the National Health Service (UK) Klinefelter’s features include:
- in babies and toddlers – weak muscles and very flexible (hypermobile) joints, learning to sit up, crawl, walk and talk later than usual, being quieter and more passive than usual, having undescended testicles, only one testicle, or a smaller penis
- in childhood – shyness and low self-confidence, problems with reading, writing, spelling and paying attention, mild dyslexia or dyspraxia, low energy levels, and difficulty socialising or expressing feelings
- in teenagers – growing taller than expected for the family (with long arms and legs), broad hips, poor muscle tone and slower than usual muscle growth, reduced facial and body hair that starts growing later than usual, small, firm testes, and enlarged breasts (gynaecomastia)
- in adulthood – inability to have children naturally (infertility), low sex drive, small, firm testes, and erection problems.
Additionally, men with Klinefelter’s may experience:
- type 2 diabetes
- weak and fragile bones (osteoporosis)
- cardiovascular disease and blood clots
- autoimmune disorders (where the immune system mistakenly attacks the body), such as lupus
- an underactive thyroid gland (hypothyroidism)
- anxiety, learning difficulties and depression – although intelligence is usually unaffected
- male breast cancer – although this is very rare
According to the Mayo Clinic, signs and symptoms may include:
- Taller than average stature
- Longer legs, shorter torso and broader hips compared with other boys
- Absent, delayed or incomplete puberty
- After puberty, less muscle and less facial and body hair compared with other teens
- Small, firm testicles
- Small penis
- Enlarged breast tissue (gynecomastia)
- Weak bones
- Low energy levels
- Tendency to be shy and sensitive
- Difficulty expressing thoughts and feelings or socializing
- Problems with reading, writing, spelling or math
Medline Plus provides even further detail, including more of the mental traits, and even the 5th finger fifth finger clinodactyly.
Now, to be fair, Joey doesn’t exhibit every single trait, but he exhibits many of them, and for several of the ones that “don’t fit” he is the exact opposite of he expectation.
For example, instead of having no body/facial hair, he went bald at 17. Instead of flat feet, he has extreme arches.
He doesn’t appear tall, but towers over both of his parents.
When I started to review these lists I had that same whirlwind feeling that I had when I found Ehlers-Danlos. I presented it to him, and it clicked deeply for him as well.
Testing??
Great. Now we had to figure out how to get him tested. Dr. Hardon clearly doesn’t see it. Dr. Bridenstine should have seen it. I’m almost certain that Dr. Wolach knew exactly what this was, and willfully refused to have that conversation with Joey.
Refusal to Help
Joey went back to Banner Endocrinology and Dr. Bridenstine had moved on. He was seen by Dr. Odeki who told Joey that he could tell just by looking at him that he doesn’t have Klinefelter’s Syndrome, and he refused to order the karyotype test.
Dr. Hardon had shown himself to be willing and receptive to helping, but not very willing to see the bigger picture. Nevertheless he was sympathetic to Joey’s account of trying to get anywhere with endocrinology, and he ordered the karyotype test.
Several weeks passed before getting the result.
Several weeks in which researching felt like jumping the gun. Several weeks in which I became totally prepared to have to start over from scratch after finding another dead end.
When the test came back, it confirmed Klinefelter’s Syndrome.
We somehow thought that figuring out what was causing it would cause some level of increased or redirected care. Not so.
Despite the fact that Klinefelter’s affects Joey’s mental state, testosterone, and almost every system in his body, Dr. Hardon told him not to get hung up on the Klinefelter’s, claiming that it only affects his T level, and doesn’t really matter.
WHAT?!?
He still refused to see the big picture. Instead of joining Joey in understanding the role an extra X chromosome has played in his bodily experience, Dr. Hardon dismissed the request as some machismatic gender dysphoria and just said “Look, you’re still a man.”
That wasn’t the question or request, but he certainly revealed his priorities in the conversation. I’m very grateful to Dr. Hardon, and still recognize that this is the border of his utility as part of Joey’s care team.
He referred Joey for genetic counseling- to the only geneticist in the state that handles such cases- the same geneticist I was referred to with the 12-18- month waiting list just to be able to make the appointment.
Joey called DAILY for a while, and I’m happy to announce that he has an appointment in June.
That’s more than 7 months from the time of diagnosis. 7+ months of just waiting to know anything of use. 7+ months without coordinated care, which is repeatedly called for in the sparse literature available about KS.
The myriad of symptoms don’t let up just because it’s not urgent to anybody else. That reality is incredibly taxing, both mentally and physically, for a person who is already in need of help.
Somehow this is how the system really works.
Changing Care
Joey pushed to be moved from Banner Endocrinology to UC Health Endocrinology (I will compare Banner and UC Health more in another post).
Dysautonomia
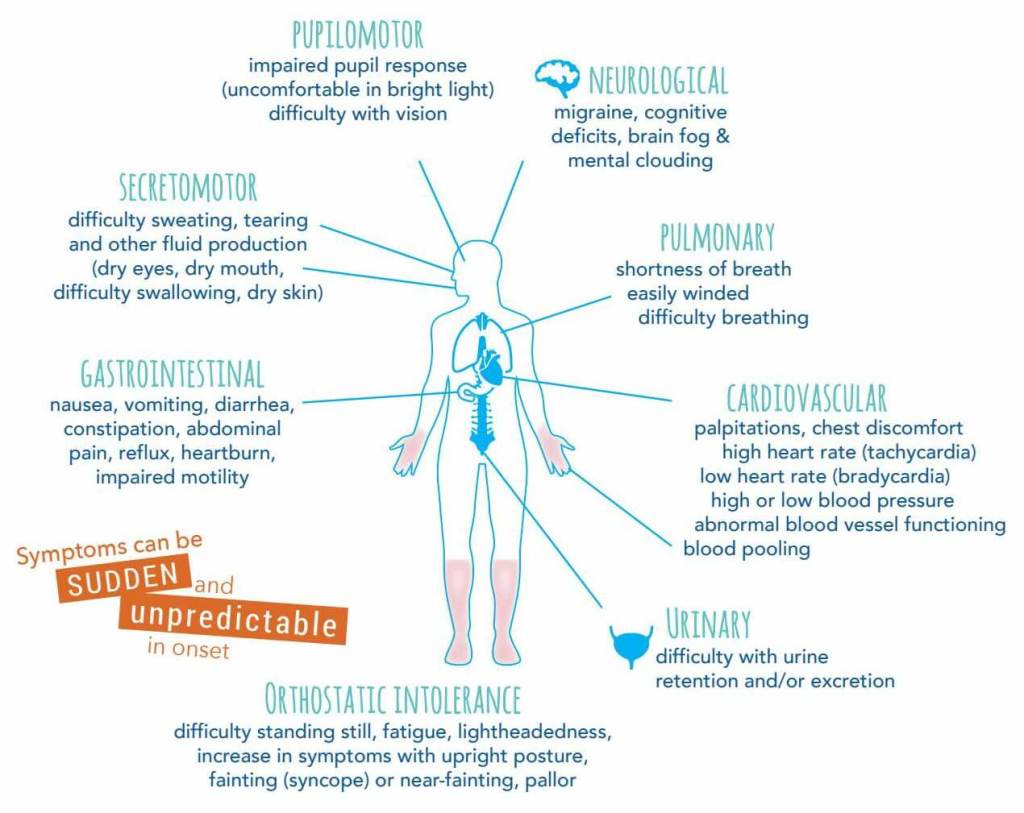
I dug into the research deep, learning all I can about the complex of symptoms I see in Joey, and that he reports to me. We discovered that he is likely Dysautonomic.
The UC Health endocrinologist was wonderful despite our nerves being wracked by the PTSD of so much medical dismissal.
Dr. Katwal reviewed the information that we had prepared, and was very willing to see the big picture. She is also willing to be a part of the team that will use a multidisciplinary approach– because she can’t work outside of her specialty.
Further Care
We now have neurology referrals for the essential tremor that continues to worsen, along with the dysautonomia.
We’re still trying to figure out how to get in to see anyone who can do mental assessments.
And so, clearly, I’ve become his care coordinator, because nobody else will despite him literally begging for help. I also had to be the diagnostician in both of our cases.
This is not health care.
There is so much wrong with this, that I’m going to have to branch out into other posts to cover it all.
Welcome to another journey of the chronically misdiagnosed and underdiagnosed.
If you have any feedback please don’t hesitate to reach out to me at ProtyusAGender@gmail.com.
Stay tuned for more information about Klinefelter’s Syndrome and Joey’s Journey to Care. Thanks for being in this with us.

What do you think?